WATTBA: Transplanted pancreatic cells edition
WATTBA, if you were wondering, stands for What A Time To Be Alive.
A Primer
When you eat food, your body converts some of that food into glucose, and that glucose is sent all over your body via your bloodstream. This is a gloriously simplified statement, but it is mostly correct, and therefore mostly harmless.
When you eat too much food (especially of the wrong kind - and the wrong kind is always the very best thing to eat), your body produces too much glucose, much more than your body needs, or is able to store efficiently. And when your blood has too much glucose in it, bad things happen. This is also mc, and therefore mh.
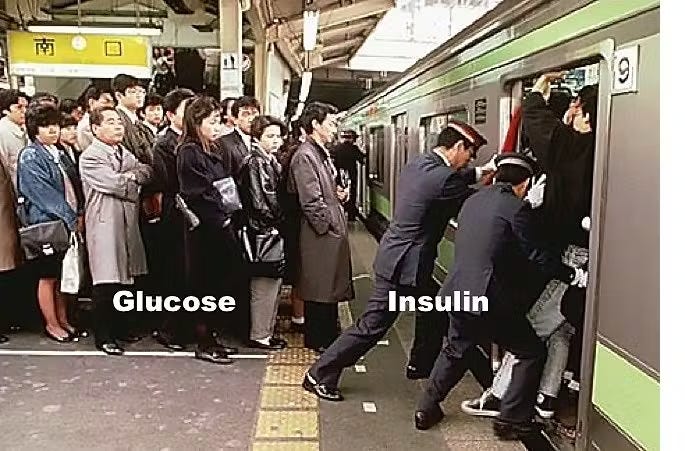
When this happens, your body releases a hormone called insulin, which goes around your body, asking cells to take in a bit more glucose, so that the problem goes away. It looks something like this:
And here's Jason Fung with a lovely explanation:
Imagine the cell to be a subway car. When the door opens, the passengers on the outside (glucose in the blood) march in a nice orderly manner into the empty subway car (cell). Normally, it doesn't really require much of a push to get this glucose into the cell (insulin gives the push).
But during insulin resistance, the problem is not that the door does not open. The problem, instead is that the subway car (cell) is already overflowing with passengers (glucose). Now the glucose outside the cell simply can't get in and is left crowded on the platform.
Insulin tries to push the glucose into the cell like the Japanese Subway Pushers, but they simply can't do it because it's full. So, it looks like the cell is resistant to the effects of the insulin, but really the problem is that the cell is already overflowing. So, the knee jerk reaction is to manufacture more insulin (pushers) to help push glucose into the cell. Which works, but only for a while.
This is, in a nutshell, what happens in Type II diabetes. Too much glucose in your blood, and your body's ability to produce enough insulin to deal with it ain't enough. There's a lot more to it, but we'll stop here for now, thank you.
Type I diabetes is worse, because the problem isn't "enough insulin", the problem is that there is no insulin. And the reason there is no insulin is because your body doesn't produce any.
And why does it not produce any? Well, it doesn't produce any because if you're suffering from Type I diabetes, your body doesn't have any islets of Langerhans. Islets of Langerhans are a tiny cluster of cells in your pancreas, whose sole job it is to make insulin. In the case of Type-I diabetes, your immune system destroys the insulin-making β-cells inside the islets, so functional insulin production drops to ~zero
No β-cells -> no insulin -> Very Big Problem.
I Mean, There's An Obvious Solution, No?
If you're not a trained biologist, there's a chance you've read so far and went, "Er, I mean, why don't you just stuff some of these islets in?"
Hell, if Elon can go and tinker about in your brain with Neuralink, how difficult can it be to get somebody else's islets of Langerhans into the patient? Eh?
Well, now, you're on the right track, and this route has been tried. But there are two important and major roadblocks. Their names are Major Histocompatibility Complex molecules, and just like Kill Bill, they come in two parts (I and II, if you were wondering).
These molecules are an integral part of your immune system, and that's the good news. These molecules are like ID cards - if your body's immune system sees the wrong set of ID cards, the card carriers are, uh, eliminated in short order.. This, of course, is the bad news.
OK, So There's A Not So Obvious Solution, Then
"Well, ok", you might say then, and maybe you'll scratch your chin pensively.
"What if we transplant the Islets of Langerhans and give some other medicine that will ask these MHC I & II fellows to go take a chill pill?"
Dr. James Shapiro, Dr. Jonathan Lakey, Dr Edmond Ryan, Dr. Gregory Korbutt, Dr. Ellen Toth, Dr. Garth Warnock, Dr. Norman Kneteman, and Dr. Ray Rajotte would have beamed approvingly at you if they were around, for you, like them, are recommending the Edmonton Protocol.
There are, however, three major problems with the Edmonton Protocol (there's always a but, isn't there?):
The islet transplants don't last forever, they last for about six years or so.
There is a very small list of willing donors (the islets can only be taken from cadavers)
Immunosuppressant drugs Are. Not. Fun.
You see, when you take drugs that tell the MHC I and II fellows to chill a little in life, they take you very, very seriously. They don't just chill about those new islets, they chill about every foreign visitor inside your body. And that means that you are susceptible to a whole other bunch of diseases.
But, hang on, fret not and worry not, because there is a new game in town. Maybe. Hopefully.
Say Hello to Sana
https://twitter.com/rtnarch/status/1937152126603395107
How do you transplant pancreatic islets with no immunosuppression needed? Well, Sana's research allows it to create islets with no MHC-I and no MHC-II at all. It's like landing up on a college campus with no ID at all, as opposed to the ID of another college.
But wait, the attentive ones among you might say. Won't the guard at the gate ask to see some ID that does belong to this particular college? Well, that's where CD47 comes in.
CD47 is a (I love this phrasing) "Don't Eat Me" signal, and I mean that quite literally. If a molecule in your body has a CD47 covering that can be understood and identified by your body's defense systems, they let you go through, no questions asked.
Have you ever tried entering a campus, a show, an office by using nothing but bravado? You hope to project that you belong, and it is so obvious, that the guard feels like a bit of a chump asking you to identify yourself. Know the feeling? CD47 is something like that.
So Sana has managed to create islets that don't have ID cards (MHC-I and MHC-II), and has a cloak of bravado (over-expressed CD47).
And they went and put these islets into a patient:
Ta-Da!!!
Six months in, said patient is doing well, and the body has accepted the islets, no problem. There are two things that are important to note, though. One, the islets were transferred into a muscle on the patient's forearm, presumably because this was easier. And two, while the islets are there, and they are producing insulin (which has been tracked my using C-peptide levels in the blood, a definitive marker of insulin production), it's a very small amount, and nowhere near enough.
But hey. Hey, hey, hey.
Yes, this is a sample size of one. Yes, it has only been six months. Yes, a lot of things could go wrong, and more experimentation is needed. Yes, we're still dependent on a very limited and very complicated source (cadavers) for the islets.
But as a proof of concept, this is as definitive as it gets. All of those factors up there are valid, and there will no doubt be many stumbling blocks. But the fact remains that we are now able to get the human body to accept islets of Langerhans from outside. Not just accept them, but to do so without making our immune system look like the monsoon session of our Parliament, where no work gets done.
If you've read thus far, and understood what I've been talking about, you should have the exact same question that I did when I reached about here: well, what else can we bung in there?
New heart muscles after a heart attack? Get malfunctioning kidneys to work well again? Knee joints? Hip joints?
Cold Water Time
I do not mean to suggest that this is all solved, and off-the-shelf replacement organs are just waiting to turn us into Ships of Theseus. But I very much do mean to suggest that this is an important medical advance, and that in terms of medical capabilities, the future just got a whole lot brighter.
Much work remains to be done, and many hurdles will pop-up, and this will take a fair bit of time. But all that being said, if you feel like popping open the bubbly, I'll agree. Pour me a glass too, while you are at it.
Better yet, make it three glasses.